AFTER PREECLAMPSIA: What do I do when my risk is not gone, but my healthcare plan is?
As a preeclampsia survivor in our PF community, you are probably well-aware that you have a higher risk for various forms of heart disease than our “normal” pregnancy peers. As one survivor said to me during this summer’s Reconnect Tour about preeclampsia and her heart health, “It ain’t over when it’s over!”
I share her concerns and frustrations. When trying to find a cardiologist for myself who understands (1) that women’s heart health is not evaluated and measured the same as men’s heart health*, and (2) that pregnancy history matters, I have found little local support. I live in a pretty well-populated part of America, with several cardiologists in town. They all look at me like I have three heads when I ask them to help evaluate my specific risk. I’ve even talked to leadership at the American College of Cardiology. There is no “directory of women’s heart specialists.” Most cardiologists (and especially primary care providers) simply don’t know what to do with preeclampsia survivors – even those of us who are aware of our long-term risk.
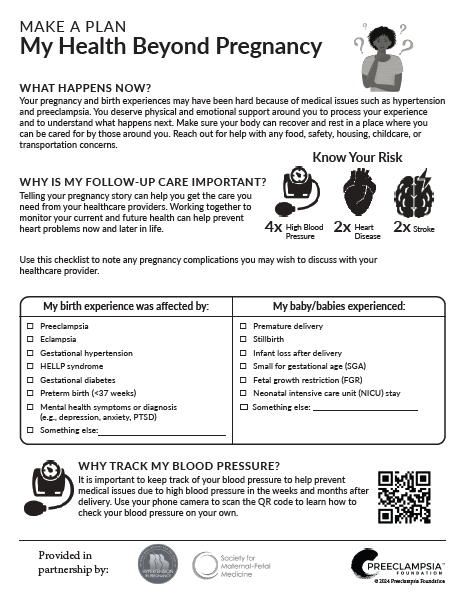
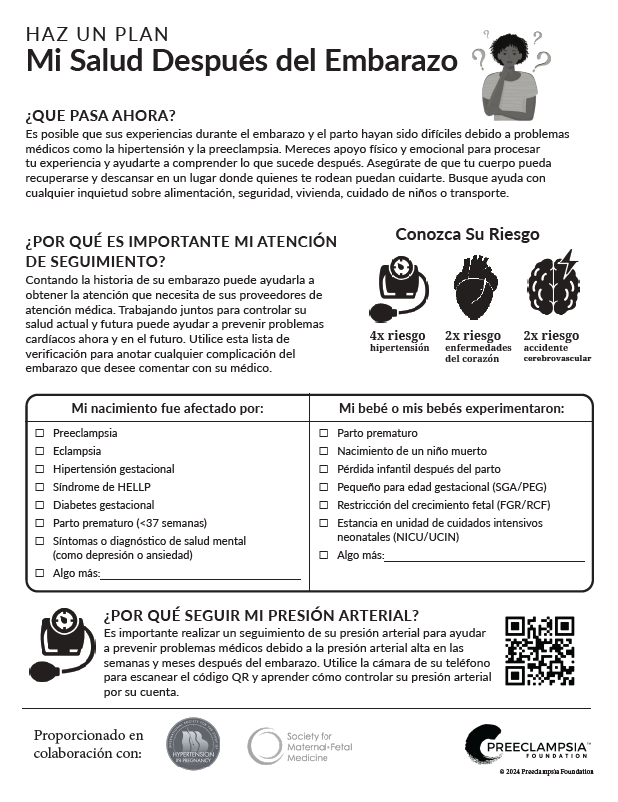
We recently asked you, our community, what you knew about long-term risk and what questions you had. Over 600 people responded, with almost 80% of you stating that you knew there was long-term risk following preeclampsia, but the most frequently raised question remained, “What specific follow-up care should I receive and who should I see for this?”
We can do better for preeclampsia survivors beyond pregnancy. I know because I’ve seen first-hand when it’s done well. While on the road this summer for the Reconnect Tour 2022, I met with academic and clinical centers of preeclampsia excellence whose leadership recognize that there is a gap between our pregnancy care and everything that happens beyond pregnancy. These have begun to put together unique “dream teams” of obstetricians and cardiologists to create postpartum clinics with a focus on health after preeclampsia.
Pregnancy is a unique stress test on the heart and blood vessels: with a 50% increase in blood volume, our hearts during pregnancy are essentially running marathons for months on end. It then takes months for our bodies to return to a new normal – and even more so if your vessels were extra taxed by high blood pressure.
Enter solutions. Many of the institutions I visited are deploying postpartum clinics that not only fill a critical healthcare gap for preeclampsia survivors, but also become a learning hub for building our medical and biological understanding of and for this unique population. We need healthcare providers who are equipped to measure, evaluate and guide our transition back to health – a process that may take months, or even years.
University of Pittsburgh cardiologist Malamo Countouris, MD, the co-director of their Postpartum Hypertension Clinic at the Magee Womens Heart Center, explained that they treat new mothers with pregnancy-related high blood pressure issues to screen for risk factors and coach them through healthy life style changes to reduce their risk of chronic hypertension and heart disease in the future.
The University of Chicago’s Dr. Tamar Polonsky presented their preventative cardiology program, emphasizing the need for specialized patient education around nutrition and exercise in a way that is accessible and not intimidating. You can learn more from Dr. Polonsky in this video.
And while I didn’t get a chance to tour the facilities, I enjoyed a private lunch with Dr. Ann Celi who runs the postpartum clinic at Brigham and Womens Hospital in Boston. Her commitment to whole-person care is inspiring. She worked closely with the Preeclampsia Foundation to produce the very popular How to Take your Blood Pressure video and continues to be a valuable partner with the PF.
Yale New Haven Health System has numerous programs they’re testing, including a large PCORI-funded program to evaluate two health care delivery models which focus on the awareness, early detection, and control of postpartum hypertension, as well as social and mental health factors known to affect maternal health. Dr. Heather Lipkind, with whom we met, said, “Poor blood pressure control, due to a lack of follow-up and identification during the postpartum period, is one of the drivers of racial inequities in maternal morbidity and mortality.” Since half of pregnancy-related deaths occur postpartum, we must look to that time period for solutions.
We believe, as do most of the hospital leaders with whom we met, that Self-Measured Blood Pressure (SMBP) is also part of the solution, particularly when incorporated with telehealth options which wisely reflect the challenges of new moms and their newborns physically attending all post-partum health visits.
As I noted in my first blog post from the Reconnect Tour, one of the hopeful and yet concerning observations I made was the problem of geography. The depth of talented doctors and nurses who are truly innovating to address gaps in diagnosis and care is remarkable – in urban areas with large teaching hospitals. But are these innovations making their way to suburban and rural parts of our country? How do we get that same care to other parts of the country – many of which face high rates of both maternal and chronic illnesses? How do we test, standardize, package, and scale these programs so that ALL preeclampsia survivors have access to lifelong health? Making virtual or telehealth visits an option has been shown to increase patient use of these specialized postpartum programs and, importantly, may be an excellent way to bridge the geographic divide that I witnessed in many of my visits.
The 8 keys to successful clinics include:
- Programs co-designed by and for the community they intend to serve;
- Engage and educate the patient while their pregnancy experience is still fresh;
- Multidisciplinary staffs that include cardiologists, maternal fetal medicine obstetricians, nutritionists, physical activity specialists, social workers and mental health support -- all of whom recognize the unique circumstances and challenges of new mothers;
- Provide patients with self-measured blood pressure (SMBP) tools and information;
- Engage community support for the new mom at the center of the program (beyond just her immediate family);
- Offer telehealth (remote) options to overcome access challenges;
- Ensure medical benefits from private and public insurers are available for a year past delivery;
- Provide a seamless hand off to the patient’s primary care provider.
All this is to say, I’m highly encouraged by the innovation of postpartum clinics that recognize and address the unique histories and risks of preeclampsia survivors. Now if we can just get the benefits of those resources to those of us not living near one of the centers of preeclampsia excellence!
*My friend and fellow advocate Carolyn Thomas writes and teaches about gender differences in heart health in her blog, Heart Sisters. I highly recommend you read it.
Related Articles

A visual approach to understand preeclampsia patient experiences from the Society for Maternal-Fetal Medicine & Preeclampsia Foundation

Doulas can help bridge the gap for any mom, but especially those most vulnerable to maternal illness and death.

Stories of our brave women and families who have been affected by preeclampsia and HELLP syndrome. Please note that due to a technical issue, we are currently fixing the images on this page.

What is Preeclampsia? Preeclampsia is a hypertensive disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least...
1732072344.png)
While the Preeclampsia Foundation has been championing patient advocacy and representation for all families affected by hypertension in pregnancy throughout our 25 year history, we recognized the uniq...

For many members of the preeclampsia, HELLP syndrome, and eclampsia community, the neonatal intensive care unit (NICU) is a life-changing part of their pregnancy and birth experience. Parents from our...

Resultados de varios estudios apoyan la hipótesis de que el estrés causado por un embarazo y parto traumáticos puede en muchas ocasiones anular la habilidad de salir adelante emoc...
As an advocate who served on the planning committee for the Foundation’s Chicago Promise Walk and 5K Run for numerous years and currently serves on the Patient Advisory Council, Jasmine Mago is...

For those who have experienced the loss of their expected pregnancy experience, the end-of-year holiday season can be a time of grieving. Grief can manifest as anger, sadness, irritability, frustratio...