1665494820.png)
Balancing Hope & Concerns: Reflections from the Road
 The pandemic hasn’t stopped everything. In some cases, it has been the catalyst for the kind of innovation that is poised to stay with us long past mandatory quarantines and telehealth visits.
The pandemic hasn’t stopped everything. In some cases, it has been the catalyst for the kind of innovation that is poised to stay with us long past mandatory quarantines and telehealth visits.
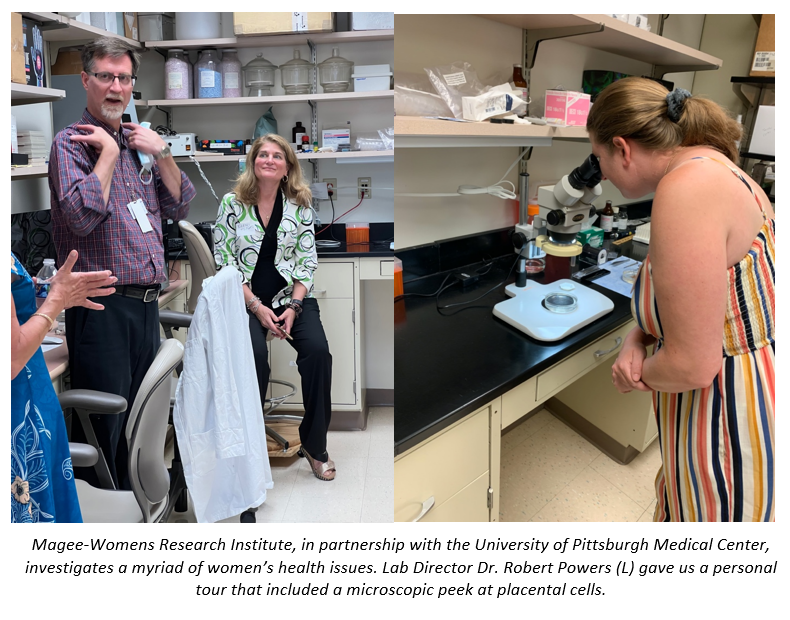
Spending two months on the road has given me in-depth and personal encounters with some of our country’s leading academic hospitals and preeclampsia research centers. Site visits to the University of Wisconsin, University of Illinois-Chicago, University of Pittsburgh Medical Center & Magee-Womens Research Institute, Yale-New Haven Health and Yale-Bridgeport Hospital, have provided a view into the problems currently being tackled by leading investigators caring for preeclampsia patients. (View the full ReConnect roadtrip itinerary.)
Hypertension monitoring and management figures prominently in much of their work. Most of these “centers of preeclampsia excellence” (my name for them, not theirs) are deploying and studying the effectiveness of home blood pressure monitoring, some with automatic readings sent to healthcare providers, and some with telehealth services to respond to high blood pressures and administer medications. While some of these initiatives were accelerated and/or put into widespread clinical use during the pandemic, most are now providing this service in the postpartum period, when the baby is no longer part of the risk assessment. I urged them forward to see this through: putting BP monitors in the hands of patients furthers their self-efficacy, just as preeclampsia education empowers mothers to name the symptoms they may feel, trust their intuition to report their concerns, and stand their ground if they have to advocate to be heard. Moms in both the prenatal AND postpartum periods could be equipped to measure and report their blood pressure, just as they are taught to look out for concerning symptoms.
I met with several site leaders of the Maternal-Fetal Medicine Units Network, one of the largest research consortia studying maternal health problems like preeclampsia, having recently completed the CHAPS trial. All agreed that this landmark study answers any remaining questions about the importance of treating even “mild” hypertension before and during pregnancy, as a way to prevent or mitigate the onset of preeclampsia for a significant percentage of women who would otherwise go on to develop the condition. While treating blood pressure alone won’t prevent preeclampsia in all women, just like aspirin isn’t a universally effective prophylactic, it has been found to be enough of a deterrent to warrant a change in management guidelines. The CHAPS trial paves the way for more aggressive blood pressure control in hospital settings, before it reaches severe levels of 160/110, as provided in current “bundle” guidelines. You can watch my Beyond the Headlines interview with the first author, Dr. Alan Tita, here [LINK]; and read the guidelines issued by ACOG and SMFM.

Beyond more aggressive anti-hypertensive treatment at or near delivery, the most pervasive question is what to do with preeclampsia survivors in the weeks, months and even years after their affected pregnancies. Leveraging their local expertise to launch clinics comprising cardiologists, internists, obstetricians and other allied healthcare professionals, these innovators are providing preeclampsia survivors a way to mitigate their subsequent cardiovascular risk. Research from the STAC trial in Wisconsin found that the riskiest days for BP spikes are up to one week postpartum, similar to findings in the other centers’ postpartum research studies. UPMC research found hypertension worsens after discharge and 50% of women hang onto their hypertension beyond the typical six week post-partum visit, adding to their heightened risk of cardiovascular diseases. This problem is even greater in Black women. Addressing their risks requires a wholistic approach including nutrition and exercise counseling, physical exams and tests, addressing extra challenges of daily living, and sometimes medication. All the remote monitoring programs were found to be feasible and acceptable to patients, certainly preferable over the current standard which expects mothers to come back to a hospital or doctor’s office a week after giving birth for a blood pressure check.

I left these visits during the first half of my Reconnect Tour 2022 feeling optimistic that the biggest problems the Preeclampsia Foundation has been shouting from our soapbox ARE being addressed by some of the smartest, most dedicated clinicians and researchers.
However, I’m also left concerned that we are just widening the gap for the majority of women in this country who are not served by these and other centers of excellence.
Most of us live, work, play and pray in small communities (or even some larger towns and cities) untouched by the bleeding edge of innovation. My stop in Hagerstown, Maryland, a picturesque town nestled in the mountains within 100 miles from two major cities but seemingly miles away from the advanced care preeclampsia patients need, reminded me that preeclampsia stories from Americana are still fraught with delays in diagnosis, dismissal of women’s concerns, and denial that rising blood pressure warrants immediate attention.
How do we bring the appropriate level of medical care, respectful attention, and vital information to the majority of our families that live, work, play and pray outside of “centers of excellence”?
Related Articles

A visual approach to understand preeclampsia patient experiences from the Society for Maternal-Fetal Medicine & Preeclampsia Foundation

Doulas can help bridge the gap for any mom, but especially those most vulnerable to maternal illness and death.

Stories of our brave women and families who have been affected by preeclampsia and HELLP syndrome. Please note that due to a technical issue, we are currently fixing the images on this page.

What is Preeclampsia? Preeclampsia is a hypertensive disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least...
1732072344.png)
While the Preeclampsia Foundation has been championing patient advocacy and representation for all families affected by hypertension in pregnancy throughout our 25 year history, we recognized the uniq...

For many members of the preeclampsia, HELLP syndrome, and eclampsia community, the neonatal intensive care unit (NICU) is a life-changing part of their pregnancy and birth experience. Parents from our...

Resultados de varios estudios apoyan la hipótesis de que el estrés causado por un embarazo y parto traumáticos puede en muchas ocasiones anular la habilidad de salir adelante emoc...
As an advocate who served on the planning committee for the Foundation’s Chicago Promise Walk and 5K Run for numerous years and currently serves on the Patient Advisory Council, Jasmine Mago is...

As a preeclampsia survivor in our PF community, you are probably well-aware that you have a higher risk for various forms of heart disease than our “normal” pregnancy peers. As one survivo...

