Beyond Pregnancy
Your emotional and physical health MATTERS.
Last Updated on March 11, 2025
A hypertensive disorder of pregnancy, including preeclampsia, eclampsia, or HELLP syndrome, can be a life-changing patient experience that goes beyond pregnancy. A history of preeclampsia places patients at higher long-term risk for:
- Chronic hypertension
- Cardiovascular disease
- Chronic kidney disease
- Stroke
- Post-traumatic stress disorder, depression, and anxiety
- Diabetes
- Venous thromboembolism
- Vascular dementia
We have to do more than just repeat that preeclampsia survivors have risks beyond pregnancy, but recognize its emotional impact, educate the affected community, and empower them with tools on how they can do to be their own best advocate beyond pregnancy.
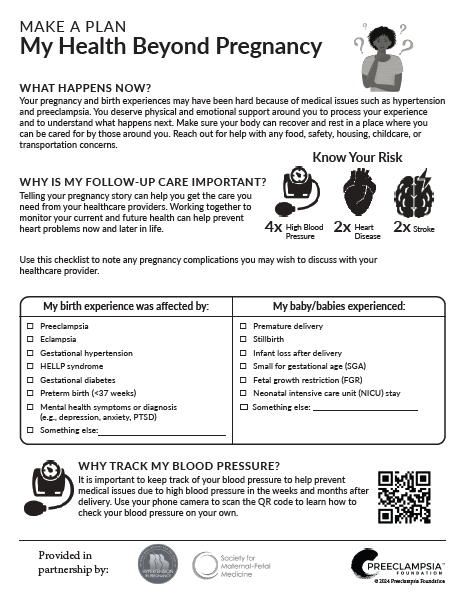
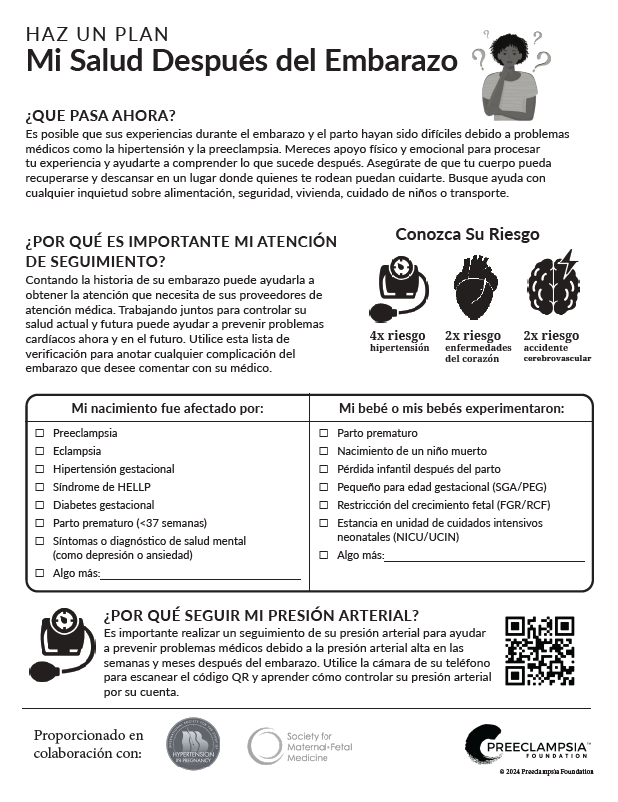
As a first step, download our "My Health Beyond Pregnancy" or "Mi Salud Después del Embarazo" printable worksheet to start the conversation with your primary care provider. Read more about the launch of version 2.0 in partnership with the International Society for the Study of Hypertension in Pregnancy and the Society for Maternal-Fetal Medicine.
FOR PATIENTS – MAKE A HEALTH PLAN THAT WORKS FOR YOU
Your pregnancy journey and birth experience may have been difficult to process because of medical complications from preeclampsia. What was supposed to be beautiful experience filled with joy was instead full of medical interventions, discomfort, and fear. This may have included more time in the hospital for you or your baby. You may have experienced complications from a premature delivery, such as a stillbirth or loss.
You are not alone. You deserve physical and emotional support around you to process your experience and to understand what happens next.
After having preeclampsia, what steps should I take?
Make a plan – forewarned is forearmed! While you cannot control the fact that you had preeclampsia, you can be empowered to make yourself heard by your care providers and to take charge of your health.
That’s where our “My Health Beyond Pregnancy” worksheet comes in – a downloadable tracking sheet that you can bring with you to your obstetrician, your general care provider, a cardiologist, or any other medical care provider that you see. This sheet was developed to help you organize your care beyond pregnancy. The worksheet helps you track important statistics like blood pressure, weight, birth outcomes, and blood work (including when it should occur) in one convenient document. It is designed to be a tool for discussing your future health, given your preeclampsia history, with your healthcare provider.
At your next regular visit, talk to your health care provider about your heart health risk or any other concerns you are having. A woman’s pregnancy can be a window to future health, yet that concept is still relatively new to the medical field.
He or she might be unaware of the link between hypertension in pregnancy and long-term heart health. If so, encourage him or her to:
- Read up on the latest guidelines from the American College of Obstetricians and Gynecologists and the American Heart Association.
- Order bloodwork to provide a baseline for your heart and kidney health
- Talk about preventative steps that you can take to maximize your health now

Patients with a history of hypertension in pregnancy should be the first ones to take and track their blood pressure at home. Whether you use a paper blood pressure log or one of many apps tracking, it is important to monitor your personal trends. If you have high blood pressure readings (140/90), verify the reading with your health care provider and discuss with him or her about any necessary medications or lifestyle changes you should make to reach your target blood pressure goal.
Watch our video on How To Take Your Blood Pressure – and be sure to #CheckKnowShare your numbers with your health care provider.
What should I do if I am feeling emotionally vulnerable?
Your pregnancy journey and birth experience may have been difficult to process because of medical complications from preeclampsia or HELLP syndrome. What was supposed to be beautiful experience filled with joy was instead full of medical interventions, discomfort, and fear. This may have included more time in the hospital for you or your baby. You may have experienced complications from a premature delivery, such as a stillbirth or loss.
Society has a way of telling moms they should feel fortunate that they are “ok” but its okay if you are not. Birth trauma is real. Many preeclampsia patients mourn this loss just like you.
Life after loss. Where do I begin?
For those who experience the unthinkable – the loss of your infant or your partner, daughter or family member to this disease, your life is forever changed. You should never have to process a grief this profound alone.
Please seek the help of a professional grief counselor to help you with this extraordinary loss. One place to start is our “Emotional Support Resources” link.
Take the First Steps toward Processing Your Traumatic Pregnancy
You deserve the emotional and psychological support needed to process your experience. You or your partner may also need some time to psychologically process your experience together particularly as it relates to your future childbearing.
Get the emotional support you need, but also pay particular attention to your physical wellbeing. Something as simple as being active and getting outdoors can positively affect your emotional health. Aim for 150 minutes of activity per week (about 30 minutes 5x a week). Try incorporating a friend, a loved one, or even your child(ren) into daily walks.

What should I do if I am unsure about having another pregnancy after my preeclampsia experience?
First, know that you are not alone in feeling unsure about having another pregnancy after experiencing preeclampsia. You and your family have been through a very traumatic experience. While having had preeclampsia in one pregnancy does place you at higher risk for preeclampsia again, repeat occurrences are often less severe. Read our article about “Trying Again After Preeclampsia” as a place to start.
Next, seek a consultation with a maternal-fetal medicine subspecialist (you can use the SMFM physician locator tool to find one in your area and read more on their special website for high-risk pregnancies).
Take your “My Health Beyond Pregnancy” worksheet with you and take notes. These subspecialists can help evaluate your risk, look for underlying health issues, and help you and your partner optimize your health for another pregnancy if you choose.
Is there anything that I can do about my heart health risk?
Absolutely! You did not cause your preeclampsia or the additional heart risk that it conveys, but you CAN take that risk seriously. Although preeclampsia survivors are at risk of developing heart disease sooner than women with normotensive pregnancies, we know that heart disease takes years to develop. That means that you can take steps now to reduce your risk.
Take the challenge to incorporate one of the following heart-health living tips into your life this May in honor of Preeclampsia Awareness Month!
Eating a diet high in fiber, vegetables, and fruits, and low in fat (the NHLBI Dietary Approaches to Stop Hypertension – or DASH – eating plan) has been proven to help lower blood pressure. Even if you don’t have high blood pressure, it will help you develop healthy eating habits and may prevent or delay your developing high blood pressure in the future. Proper diet and exercise can reduce your risk factors for heart disease.
Check out this fabulous postpartum “Nutrition after Preeclampsia” handout from Brigham and Women's Hospital, which focuses on easy-to-implement shifts for your heart health.

Research continues to show that firsthand and secondhand smoke are dangerous. Tobacco raises blood pressure and damages blood vessels immediately. Preeclampsia survivors should avoid the extra risk!

It is important to emphasize that not all women who develop preeclampsia or hypertension are overweight. Nor do all women who are overweight develop preeclampsia. Your body weight (and what is called your body mass index or BMI) are just one sign that helps your provider get a full picture of your overall health. It does not have to be your first priority - it is just one risk factor that can be changed.
Body mass index (BMI) is your body weight relative to your height. A healthy BMI is between 18.5 and 25. A BMI greater than 25 may increase your risk for heart disease and other long-term health conditions, which is why your care provider tracks your weight. If your BMI is high, talk to your health care provider about different ways to safely lose weight.
Underweight = <18.5
Normal weight = 18.5–24.9
Overweight = 25–29.9
Obesity = BMI of 30 or greater
Calculate your BMI with this NHLBI tool. Your goal should always be to stay active and eat a healthy diet to protect your heart!
What if my healthcare provider doesn’t take my concerns seriously?
Encourage him or her to access the resources listed below for providers. You can also always seek a second opinion, or follow-up with a specialist.
FOR PROVIDERS – BUILD AN OPTIMAL CARE PLAN BASED ON PREVENTION
Changing the health outcomes of preeclampsia patients cannot be done without a positive patient-provider partnership. We have numerous resources for health care providers to optimize their patients’ pregnancy and long-term health, starting with our “Best Practices” page.
What do I need to know about preeclampsia and the risk for long-term health?
- Take some time to familiarize yourself with the most recent American Heart Association Guidelines on hypertension in pregnancy and heart health.
- Listen to your patient when she expresses concerns with any aspect of her wellbeing.
- Connect her with further resources when she needs them. That includes recognizing that mental health resources are essential for processing a traumatic pregnancy experience.
- Make sure your patient’s pregnancy history is captured in their ongoing medical records and shared with any other providers in her care network. So often they are not, and providers and patients may not think to ask or share. The significance of preeclampsia in a patient record is important to her future health.
- Ensure transition of care should a patient’s postpartum blood pressure readings not be under control. Help her to know with whom she should follow-up.
- Utilize patient education materials like the “My Health Beyond Pregnancy” tool to educate and empower your patient beyond pregnancy.
- Encourage your patient to track her blood pressure at home, making sure she understands what numbers she should report and to whom. Learn more about the Preeclampsia Foundation Cuff Kit® program to assist.
You have an important role in ensuring the long-term health of your patients. Help educate and empower your patients on the link between preeclampsia and long-term health beyond pregnancy!
Related Articles

A visual approach to understand preeclampsia patient experiences from the Society for Maternal-Fetal Medicine & Preeclampsia Foundation

Meghan Markle is opening up about her experience with postpartum preeclampsia in the debut episode of her new podcast, Confessions of a Female Founder. In the episode with her first guest and clo...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...

Recently, I came across a social media post calling attention to the global maternal health crisis from a Black woman’s perspective. Someone responded to the post asking, “What’s rac...

August 22, 2023 – Melbourne, FL –– Preeclampsia survivors and their supporters will hit the pavement with a purpose on Saturday, August 26, as part of the fourth annual Promise Walk...
As an advocate who served on the planning committee for the Foundation’s Chicago Promise Walk and 5K Run for numerous years and currently serves on the Patient Advisory Council, Jasmine Mago is...