
Last Updated on April 07, 2025
Accelerating the Development and Adoption of Biomarkers
A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction. Sadly, healthcare providers are still struggling to diagnose the syndrome of preeclampsia and stratify women's risks using antiquated tools and schemes of the 19th century. We must do better!
The Preeclampsia Foundation has advocated for the development and adoption of biomarkers for over a decade by bringing together leaders in research, industry, regulatory bodies, policy makers, professional societies, and eventually payers to engage and address this call to action, remove barriers and accelerate the development and adoption of biomarkers to improve screening and diagnosis of hypertensive and placental disorders of pregnancy.
What are biomarkers?
Biomarkers are powerful laboratory tools that can be used to detect or predict illness before symptoms begin. They are often measured from a person's blood, bodily fluids, or tissues. These unique biological products are found throughout the body. Blood pressure, urine tests, and blood work are a few biomarkers that give healthcare providers information about pregnancy health. The research into preeclampsia biomarkers has found that pregnant patients who go on to develop preeclampsia have different levels of certain biomarkers. Some relate to the growth of the placenta, some related to the body's reaction to inflammation, and some may even be genetic. There are several important benefits to introducing biomarkers into the fight against preeclampsia:
- Screening pregnant women during the first trimester for pre-symptomatic disease to enable interventional research studies, accelerating progress toward a cure;
- Determining disease severity and risk stratifying women to improve disease management, such as timing of delivery;
- Reducing costs associated with short and long term medical care by eliminating unnecessary testing and surveillance[i];
- Most importantly, saving the lives and well-being of mothers and their babies.
Which biomarkers are relevant to the diagnosis of preeclampsia?
Clinically relevant biomarkers of preeclampsia can be divided into placental, inflammatory, endothelial and metabolic categories[i]. A few promising biomarkers include Placenta Growth Factor (PlGF) which is involved in the modulation of the placental and maternal vascular system[ii], soluble FMS-like tyrosine kinase-1 receptor (sFlt-1) which antagonizes blood vessel formation and promotes endothelial dysfunction[iii], asymmetric dimethylarginine (ADMA), which interferes with nitric oxide production and leads to abnormal vascular function[iv], Congo Red, a test of protein-folding abnormalities in the urine of preeclamptic women[v], RNA signatures, and others. Combined with usual clinical and ultrasound surveillance during pregnancy, these biomarkers have been shown to diagnose preeclampsia and predict adverse outcomes with an even greater accuracy than traditional tests[vi],[vii], and some have even been shown to reduce medical costs associated with evaluations of suspected preeclampsia[viii].
Where is the FDA on the use of biomarkers?
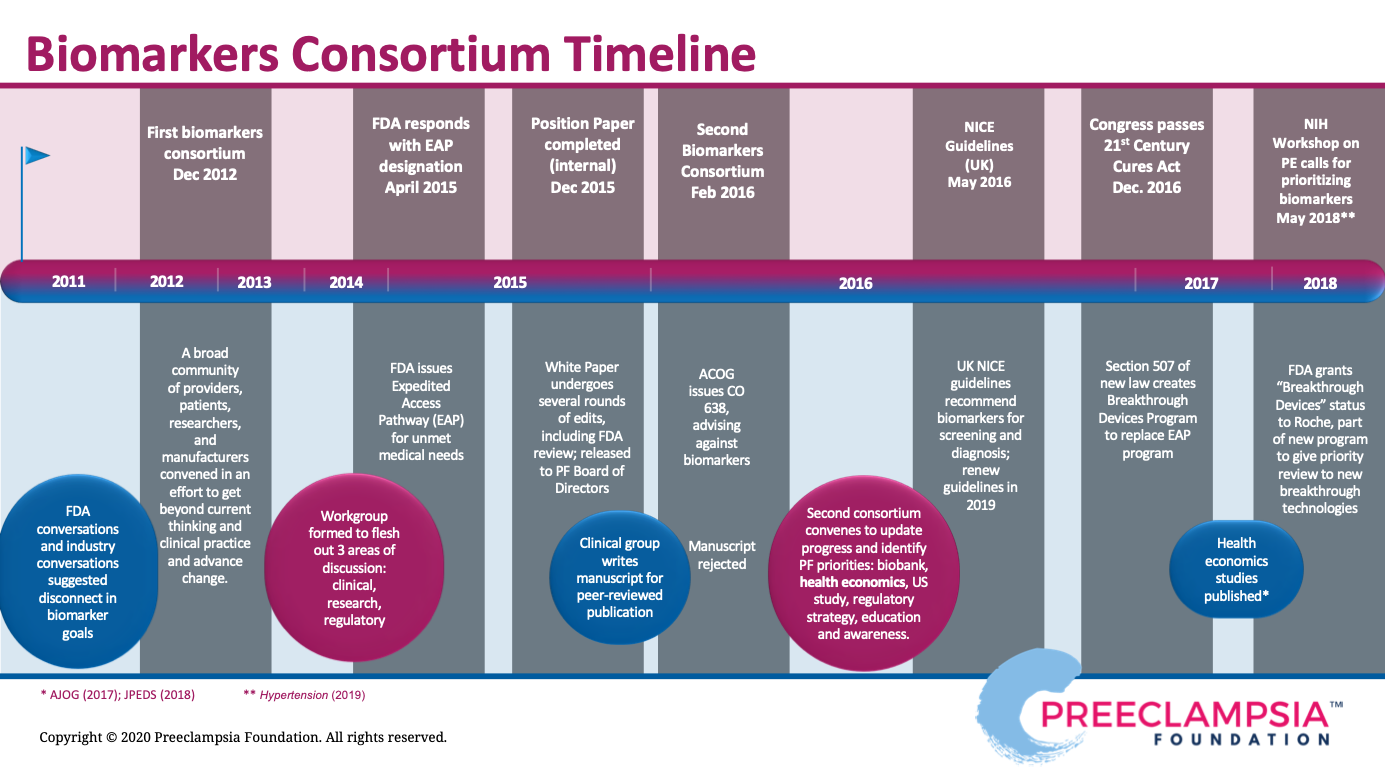
Efforts to bridge the gap between biomarker research and widespread clinical use led to the Preeclampsia Foundation hosting two biomarker consortia, in 2012 and 2016. An interdisciplinary team of experts convened to debate the current state of the biomarker field, present challenges, such as regulatory hurdles, define the need through both clinical and patient perspectives, and develop recommendations to move forward. The Food and Drug Administration (FDA), which regulates most diagnostic tools like biomarkers, participated in our meeting. Detailed findings of the consortia proceedings are summarized in our 2012 Report to Stakeholders and our 2016 Meeting Proceedings. As a result of these dynamic conversations, the FDA recognized some tests may provide substantial improvement over currently available clinical and diagnostic testing to diagnose preeclampsia and, hence, made an expedited review and approval process available to manufacturers pursuing commercial development.
In 2023, the first-ever FDA-approved test for preeclampsia was approved, which measured Placental Growth Factor (PlGF) plus and soluble FMS-like tyrosine kinase-1 receptor (sFlt-1) via a blood serum test to aid in clinical management of preeclampsia. The intended use of the test is for hospitalized patients between 23 and 35 weeks' gestation with either diagnosis of a hypertensive disorder of pregnancy or a suspicion of preeclampsia. This is a prognostic test for risk stratification, to help obstetricians determine what patient may need immediate intervention, and what patients may benefit from continued close monitoring. Another FDA-approved test for the PlGF/sFlt-1 ratio was launched in 2025.
Biomarkers are said to be the first major step in the U.S. to really help our obstetricians and clinical colleagues identify groups of patients who are at high risk for adverse outcomes and differentiate them from patients who are at low risk for adverse outcomes. Those with lower risk can potentially prolong pregnancy, thereby reducing planned prematurity that comes with preterm delivery that is often needed with the strong suspicion of severe preeclampsia.
You can help. Read the full statement below, or print it out from here, and add your voice to the growing number of advocates speaking up about the importance of molecular biomarkers by signing our petition for change.
No Time to Wait: Women Need Accurate Tests for Preeclampsia Now
A Call To Action
It is with great urgency that we call upon leaders in research, industry, regulatory bodies, policy makers, professional societies, and payers to engage and address this call to action, removing barriers and accelerating the development and clinical adoption of biomarkers for preeclampsia.
Preeclampsia is a heterogenous maternal syndrome recognized ultimately by the development of high blood pressure and multi-organ dysfunction or injury. Its clinical presentation can be quite varied and confusing: elevated BP may precede or follow proteinuria, other symptoms may be obscured; its onset may be gradual, quite sudden, or even present postpartum. It is the most common severe obstetrical complication in the U.S.[i], affecting 2 to 8 percent of pregnancies, and leading to multiple adverse maternal outcomes including seizure, stroke, heart disease, and death, as well as neonatal outcomes that include growth restriction, preterm birth, and death[ii],[iii]. The estimated cost of preeclampsia in the United States was $2.18 billion dollars in 2012[iv], the average preeclamptic pregnancy cost three times more than normotensive pregnancies[v], and the incidence of preeclampsia – especially its severe variants – has been increasing[vi], underscored by the unacceptable disparities we are seeing in both higher prevalence and worse outcomes amongst Black and American Indian/Alaskan Native women[vii][viii]. It has now been over 100 years since the term ‘preeclampsia’ was first coined to define the syndrome of hypertension, proteinuria and edema[ix] – clinical endpoints that have not markedly changed, and yet still the cause of the disease remains elusive, hampering efforts to predict, diagnose, and manage this scourge of pregnancy. Clearly, we must do better.
A key component needed in the fight against preeclampsia, and perhaps the most urgently needed, is the development of tests for simple, rapid, and accurate diagnosis and prediction. Sadly, health care providers are still struggling to diagnose the syndrome of preeclampsia and stratify women’s risks using antiquated tools and schemes of the 19th Century. Blood pressure, proteinuria, maternal symptoms, and basic blood chemistries are highly variable, nonspecific, and poorly predictive of outcome. The resulting diagnostic uncertainty is pervasive and shameful – rare or atypical cases are overlooked with potentially devastating consequences, while a great many unaffected patients are subjected to worrisome, repetitive, and wasteful surveillance or possibly even to unnecessary iatrogenic delivery. Rapid, reliable and clinically useful biomarkers for preeclampsia are urgently needed as decision aids to improve pregnancy outcomes[x].
Biomarkers are powerful laboratory tools that can be used to detect or predict pathology before symptoms, such as elevated blood pressure, are present. These unique biological products are found throughout our body and may be quantifiable by a simple blood, urine, or even a saliva test at various points in the disease process. There are several important benefits to introducing biomarkers into the fight against preeclampsia: 1) Screening pregnant women for pre-symptomatic disease to enable interventional research studies, accelerating progress toward therapeutic drugs or biologics; 2) Determining disease severity and risk stratifying women to improve surveillance and management, such as timing of delivery; 3) Reducing costs associated with short and long term medical care by eliminating unnecessary testing and surveillance[xi]; 4) and most importantly, saving the lives and well-being of mothers and their babies.
Clinically relevant biomarkers of preeclampsia can be divided into placental, inflammatory, endothelial and metabolic categories[xii]. A few promising biomarkers include Placental Growth Factor (PlGF) which is involved in the modulation of the placental and maternal vascular system[xiii], soluble FMS-like tyrosine kinase-1 receptor (sFlt-1) which antagonizes blood vessel formation and promotes endothelial dysfunction[xiv], asymmetric dimethylarginine (ADMA), which interferes with nitric oxide production and leads to abnormal vascular function[xv], Congo Red, a test of protein-folding abnormalities in the urine of preeclamptic women[xvi], and others. Combined with usual clinical and ultrasound surveillance during pregnancy, these biomarkers have been shown to diagnose preeclampsia and predict adverse outcomes with an even greater accuracy than traditional tests[xvii],[xviii], and some have even been shown to reduce medical costs associated with evaluations of suspected preeclampsia[xix].
In 2015, the American College of Obstetricians and Gynecologists (ACOG) released a committee opinion stating that, although commercial tests were available to predict preeclampsia during the first trimester, there was a lack of evidence supporting their use clinically10. Since then, ongoing research studies have further refined biomarker strategies, which are now capable of predicting over 75 percent of cases of preterm preeclampsia with a low false positive rate of 10 percent[xx] and others which have led to effective ‘rule out’ strategies[xxi],[xxii]. In other countries, serum biomarkers have already been adopted for clinical use and incorporated into management guidelines[xxiii].
Efforts to bridge the gap between biomarker research and widespread clinical use led to the Preeclampsia Foundation hosting two biomarker consortia, in 2012 and 2016. An interdisciplinary team of experts convened to debate the current state of the biomarker field, present challenges, such as regulatory hurdles, define the need through both clinical and patient perspectives, and develop recommendations to move forward. Detailed findings of the consortia proceedings are summarized in our 2012 Report to Stakeholders and our 2016 Meeting Proceedings. As a result of these dynamic conversations, the FDA recognized some tests may provide substantial improvement over currently available clinical and diagnostic testing to diagnose preeclampsia and, hence, made an expedited review and approval process available to manufacturers pursuing commercial development.
This designation and other key milestones in the evolution of the biomarker field are illustrated in Figure 1. As U.S. policymakers look to expand beyond legislative efforts to support cures and therapy breakthroughs, they should consider ongoing regulatory reforms that will allow expedited approval for new screening tests, coverage, and clinical screening guidelines. Professional societies must encourage the use of these important decision aids as clear markers of placental dysfunction.
The Preeclampsia Foundation, a patient advocacy organization, represents the nearly 300,000 pregnant women per year affected by hypertensive disorders in the US and Canada. Its purpose is to reduce the burden of preeclampsia and related complications by educating, supporting, and engaging the affected community, improving healthcare practices, and finding a cure. As such, the Preeclampsia Foundation is a strong advocate of biomarker research and clinical utilization. The Foundation has extended its support of biomarkers by awarding biomarker-based research grants, using patient surveys to demonstrate the importance of biomarkers to preeclampsia survivors, and encouraging industry to engage in biomarker development.
The status quo is inadequate. It is time to move to the molecular era. Biomarker studies and clinical adoption must be prioritized and accelerated if we are going to save the lives and improve health outcomes of preeclamptic mothers and their babies. It is with great urgency that we call upon leaders in research, industry, regulatory bodies, policy makers, professional societies, and eventually payers to engage and address this call to action, removing barriers and accelerating the development and adoption of biomarkers to improve screening and diagnosis of hypertensive and placental disorders of pregnancy.
REFERENCES
[i] O'Gorman N (2016). Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 11-13 weeks gestation. Am J Obstet Gynecol, 214:103 e101-103 e112.
[ii] Shih T (2016). The Rising Burden of Preeclampsia in the United States Impacts Both Maternal and Child Health. Am J Perinatol, 33:329-338.
[iii] English F (2015). Risk factors and effective management of preeclampsia. Integr Blood Press Control. 2015; 8: 7–12.
[iv] Stevens W (2017). Short-term costs of preeclampsia in the United States health care system. Am J Obstet Gynecol, 217:237-248 e216.
[v] Hao J (2019). Maternal and Infant Health Care Costs Related to Preeclampsia. Obstet Gynecol, 1227-1233.
[vi] Ananth CV (2013). Pre-eclampsia rates in the United States, 1980-2010: age-period-cohort analysis. BMJ, Nov 7;347:f6564.
[vii] Johnson JD (2020). Does race or ethnicity play a role in the origin, pathophysiology, and outcomes of preeclampsia? An expert review of the literature [published online ahead of print, 2020 Jul 24]. Am J Obstet Gynecol. 2020;S0002-9378(20)30769-9.
[viii] Tucker MJ (2007) Black-White disparity in pregnancy-related mortality from 5 conditions. Am J Public Health. 2007; 97:247-251.
[ix] Webster J (1903). A Text-Book of Obstetrics. Philadelphia: Saunders.
[x] Li R (2017). Health and economic burden of preeclampsia: no time for complacency. Am J Obstet Gynecol, 217:235-236.
[xi] Schnettler WT (2013). Cost and resource implications with serum angiogenic factor estimation in the triage of pre-eclampsia . BJOG, Sep;120(10):1224-32.
[xii] Eastabrook G (2018). Preeclampsia Biomarkers: An assessment of maternal cardiometabolic health. Pregnancy Hypertens, 13:204-213.
[xiii] Chau K (2017). Placental growth factor and pre-eclampsia. J Hum Hypertens, 31:782-786.
[xiv] Maynard SE (2003). Excess placental soluble fms-like tyrosine kinase (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest, 111:649-658.
[xv] Yuan J (2017). Circulating asymmetric dumethylarginine and the risk of preeclampsia: a meta-analysis based on 1338 participants. Oncotarget, 8:43944-43952.
[xvi] Rood KM (2019). Congo Red Dot Paper Test for Antenatal Triage and Rapid Identification of Preeclampsia. EClinicalMedicine. 2019;8:47-56.
[xvii] Duhig KE (2019). Placental growth factor testing for suspected pre‐eclampsia: a cost‐effectiveness analysis. BJOG, Oct;126(11):1390-1398.
[xviii] Barton JR (2020). PETRA Trial. Placental growth factor predicts time of delivery in women with signs or symptoms of early preterm preeclampsia: a prospective multicenter study. Am J Obstet Gynecol, Mar;222(3):259.e1-259.e11.
[xix] Duckworth S (2016). Placental Growth Factor (PlGF) in Women with Suspected Pre-Eclampsia Prior to 35 Weeks' Gestation: A Budget Impact Analysis. PLoS One, Oct 14;11(10):e0164276.
[xx] O'Gorman N (2017). Accuracy of competing-risks model in screening for pre-eclampsia by maternal factors and biomarkers at 11-13 weeks' gestation. Ultrasound Obstet Gynecol, June;49(6):752-755. Erratum in: Ultrasound Obstet Gynecol. 2017 Dec;50(6):807.
[xxi] Zeisler H (2016). Predictive Value of the sFlt-1:PlGF Ratio in Women with Suspected Preeclampsia. N Engl J Med. 2016;374(1):13-22.
[xxii] Cerdeira AS (2019). Randomized Interventional Study on Prediction of Preeclampsia/Eclampsia in Women With Suspected Preeclampsia: INSPIRE. Hypertension. 2019;74(4):983-990.
[xxiii] NICE (2016). PlGF-based testing to help diagnose suspected pre-eclampsia (Triage PlGF test, Elecsys immunoassay sFlt-1/PlGF ratio, DELFIA Xpress PlGF 1-2-3 test, and BRAHMS sFlt-1 Kryptor/BRAHMS PlGF plus Kryptor PE ratio). Retrieved from National Institute for Health and Care Excellence: https://www.nice.org.uk/guidance/dg23
Related Articles

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

As a first step to address the need for self-monitored blood pressure, the Preeclampsia Foundation started providing the Cuff Kit® in June 2020 to women at highest risk of developing preeclampsia and...

Every woman should be able to check her own blood pressure at home.

Order our Ask About Aspirin Rack Card. Aspirin can prevent the formation of blood clots. This can make aspirin useful in treating or preventing some conditions like heart attacks and st...

Women who have had preeclampsia have three to four times the risk of high blood pressure and double the risk for heart disease and stroke: ensure they get follow-up care beyond pregnancy.

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...
1732072344.png)
While the Preeclampsia Foundation has been championing patient advocacy and representation for all families affected by hypertension in pregnancy throughout our 25 year history, we recognized the uniq...

Washington, DC – April 11, 2024 – On April 10, one day before the start of Black Maternal Health Week, the Preeclampsia Foundation in partnership with Thermo Fisher Diagnostics held a Hill...

Recently, I came across a social media post calling attention to the global maternal health crisis from a Black woman’s perspective. Someone responded to the post asking, “What’s rac...


